
Detailed Semen Analysis
What is a detailed semen analysis?
The test involves the microscopic examination of semen to assess the concentration, motility and the morphology of the sperm against the 2010 World Health Organisation reference values. In addition to this we also look for the presence of anti-sperm antibodies which may affect mobility of the sperm.
Sperm Concentration
This is also known as ‘sperm count’ and is a measure of how many million sperm are present in each mL of your semen sample. The World Health Organisation suggests that a normal semen sample should contain at least 15 million sperm per mL.
Total Count
This indicates the total number of sperm in your ejaculate calculated using the volume and the sperm concentration. The World Health Organisation suggests that a normal semen sample should contain at least 39 million sperm.
Progressive Motility
This indicates the percentage of sperm in your sample which are swimming in a forward manner (progressively motile) and graded on their speed. The world Health Organisation suggests that a normal semen sample should contain at least 32% progressively motile sperm.
Normal Forms
Also known as sperm morphology, this is a measure of the shape and size of the sperm in your sample and is reported as a ‘normal’ percentage. The World Health Organisation suggests that a normal semen sample should contain at least 4% normal forms.
Anti-sperm Antibodies
These can occur when the body’s immune system launches an attack on your sperm. The antibodies may cause the sperm to stick together (agglutinate) or disrupt their ability to swim or impair their fertilising ability. They are rare but commonly occur after a vasectomy reversal or severe groin injury or operation. Greater than 40% agglutination is considered significant.
Enhanced Semen Analysis
The Enhanced Semen Analysis includes everything offered in the Detailed Semen Analysis along with an additional test to measure your fertility potential. This additional test is known commercially as MiOXSYS and is used to measure oxidative stress. High levels of oxidative stress can affect your sperm’s ability to function normally and can cause DNA fragmentation. This can lead to delayed time to conception, suboptimal semen parameters and unsuccessful IVF outcomes.
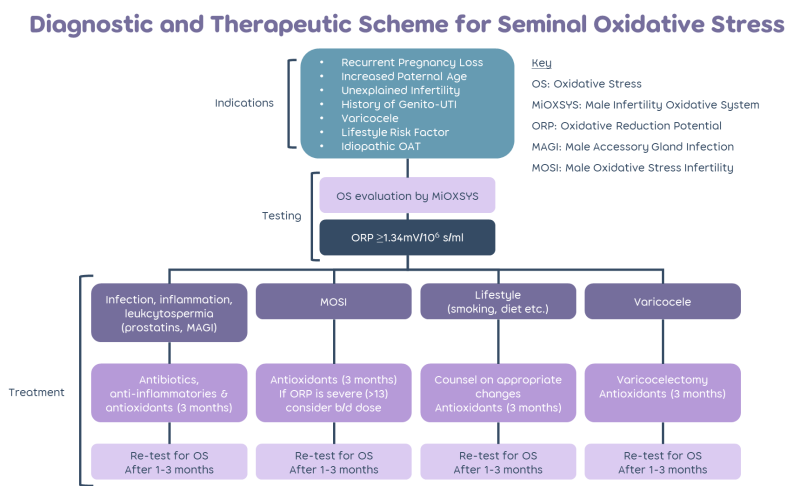
Oxidative stress can happen when an imbalance occurs between the presence of oxidants (such as reactive oxygen species) and the body’s ability to detoxify them or repair the damage caused by them. MiOXSYS works by measuring this balance (known as the static oxidation-reduction potential).
If the test reveals an imbalance, your clinician should be able to guide you on ways to try and restore the balance. This may include further tests to check for infection or the presence of a varicocele or guidance on how to improve your lifestyle. It may be possible to treat oxidative stress with a course of antioxidants however it is important to discuss this with your clinician to avoid causing an imbalance the other way. Booking a retest after making these changes will determine if an improvement has been made.
MiOXSYS may be useful for patients who have experienced recurrent pregnancy loss, have an increased paternal age, unexplained infertility, a history of genito-urinary tract infections, varicocele, lifestyle risk factors or a suboptimal semen analysis.
Enhanced Plus Semen Analysis
The Enhanced Plus Semen Analysis includes everything offered in the Enhanced Semen Analysis along with an additional test to assess DNA Fragmentation.
Although a semen analysis provides an idea of the amount of moving, normal looking sperm in your sample, a DNA Fragmentation test provides information about what is going on inside those sperm. A high level of DNA damage may lead to delayed time to conception, unsuccessful IVF outcomes and an increased risk of miscarriage.
The Exact tests, powered by SpermComet technology are performed offsite at the Examen Laboratory in Belfast. Your sample will be frozen and shipped using a special container to ensure your sperm remain at the correct temperature. Three report types are available so you can select the one which best reflects your situation.
Exact Fertility – select this test if you are still at the early stages of your investigations.
Exact IVF – this may be useful if your sperm have been identified as suitable for IVF based on the results of a detailed semen analysis. Identification of high levels of DNA fragmentation may mean that ICSI could be a better treatment choice.
Exact Miscarriage – if you have a history of sporadic or recurrent miscarriage, this may be useful to identify if sperm DNA damage could be a contributing factor.
If the test reveals a high level of DNA fragmentation, your clinician should be able to guide you on what this means. If the Enhanced Plus Semen Analysis also revealed a high level of oxidative stress, it is possible that this may be a cause of the DNA damage. Your clinician may want to undertake further tests to check for infection or the presence of a varicocele. They may also discuss how you can make lifestyle changes which may improve your results. If you have already decided to embark on fertility treatment, the results may also help to decide whether IVF or ICSI is right for you.
The test can usually be carried out on a single sample alongside the Detailed Semen Analysis and MiOXSYS. Although results for most of the tests should be available in 2-3 days, results for the DNA Fragmentation test can take around 3 weeks.
Producing your sample for analysis
In order to assess sperm at maximum quality please abstain (i.e. do not have sexual intercourse or masturbate) for 2-3 days before producing the sample. The sperm sample should be produced by masturbation into a special container (provided). The laboratory assessment of the quality of semen is a vital factor in fertility. We appreciate that being asked to produce a semen sample to order for the purpose of investigation may be difficult and embarrassing.
Please carefully note the following:
- Most of the sperm in an ejaculate is in the first portion, therefore if you collect the sample by interrupting intercourse, it is likely that this will be lost, and we will diagnose a problem, which does not exist.
- Please do not produce samples into condoms for analysis, as these contain spermicides that destroy sperm.
- Should some of the ejaculate fail to enter the container please do not submit that sample for analysis.
- We would recommend that you wash yourself with soap and water.
- If your sample is produced off site, it is important that semen samples are analysed quickly after production, as sperm begin to die quite rapidly outside the body. Deliver your sample as quickly as possible, at most within an hour of production.
- Keep the sample warm by carrying it upright in an inside pocket, but not keeping it too hot. Please label the container CLEARLY with your name and date of birth, and the date and time the sample was produced.
- The result should be available within a few days of the test. Occasionally the test needs to be repeated if the results are abnormal.
If your sample is produced off site, it is important that semen samples are analysed quickly after production, as sperm begin to die quite rapidly outside the body. We request samples are delivered to the clinic with one hour of production.
Results should be available within a few days of the test. Occasionally the test needs to be repeated if the results are abnormal.

Frequently Asked Questions
My sample volume doesn’t look as much as normal?
This is a common concern but is usually needless. The average ejaculate volume is about 2.0ml which is less than half a teaspoon or around 4mm depth in the pot.
Why has my sample gone runny?
This is perfectly normal and is called liquefaction. When a sample is first produced it is characteristically thick and globular. Between 5-60 minutes after production, this coagulum is broken down to create a runny fluid.
How can I improve my sperm test result?
Unfortunately, there is no simple answer to this question. General lifestyle changes which may improve things include wearing loose fitting underwear, taking showers instead of long hot baths, not smoking and keeping alcohol intake to a minimum. Some men do find that taking vitamin and mineral supplements help but if you have a healthy and varied diet this shouldn’t be necessary.
What happens if my results are sub-optimal or abnormal?
We would suggest that you have a repeat sample to confirm or refute the original findings. Although millions of sperm are produced by the testes every day, for an entirely new batch of sperm to be ejaculated a complete cycle of spermatogenesis (sperm production) needs to occur. This takes around 3 months. By waiting this long between tests we can rule out any temporary disruptions to sperm production which may have been caused for example by a bout of illness or stress.
If this confirms that your sperm production or quality is sub-optimal or abnormal, it would be advisable to speak to a Fertility Specialist. A physical examination, hormone and genetic tests may also be required.
What causes sub-optimal or abnormal results?
The causes of male infertility may be hormonal, genetic or physical. Exposure to certain chemicals and infections or illnesses could also hamper male fertility. However, in most cases no obvious cause is found. Sometimes, if the sperm count is borderline or slightly low, some of the following factors may be worth considering:
Was the sample ideal? Was it taken to the laboratory in time? Was it kept warm? Cooling the sample or a delay in getting it to the laboratory can alter the number of active sperm and give a false result.
It is often advised for men who have a low sperm count to wear loose fitting underpants and trousers and to avoid very hot baths, saunas, long distance cycling etc. This aims to keep your testes slightly cooler than the rest of your body, which is thought to be good for sperm production. While it is not clear whether these measures improve a sperm count, but they seem to be sensible.
Smoking can affect the sperm count. If you smoke, you should stop completely for optimum sperm production.
Excessive alcohol consumption and binge drinking may interfere with optimum fertility. Reducing intake may improve fertility.
Most drugs and medicines do not interfere with sperm production, but some may do. These include: sulphasalazine, nitrofurantoin, tetracyclines, cimetidine, colchicine, allopurinol, some chemotherapy drugs, cannabis, cocaine, and anabolic steroids. If you have a low sperm count, tell us if you take any drugs or medicines regularly.
What can be done if male factor infertility is diagnosed?
Problems with male infertility can sometimes be improved by changes in lifestyle, diet or by taking vitamins. However, because sperm takes at least 3 months to develop we have to wait a while to see if there are any improvements.
In other cases, sophisticated fertility treatment may be required. The most successful of these is a form of IVF treatment called “Intracytoplasmic sperm injection” (ICSI). ICSI is the process whereby a sperm is injected directly into an egg and can be carried out even when there are very few sperm present. If it is thought there may be male factor infertility may be due to a blockage, you may be referred for Surgical Sperm Retrieval (SSR).
It is useful to remember that in many cases even if the sperm count is low or quality is poor, conception could still occur naturally, so don’t give up trying.




