What does FET involve in IVF
Summary of Frozen Embryo Transfers (FET)
- Modern freezing techniques allow embryos to be safely frozen following IVF or ICSI treatment
- These embryos can stored and transferred to your womb at an appropriate time
- Frozen embryo transfers have comparable success rates to those with fresh embryos
How do you freeze embryos?
Embryos are frozen on day 5 or 6 of development once they have reached the blastocyst stage. They are frozen using a ‘flash-freezing’ method known as Vitrification. This involves moving a blastocyst through a series of protective solutions, using very precise timings, and instantly cooling to -196oC in liquid nitrogen. Each blastocyst is stored in an individual, sealed and labelled straw.
How do you thaw embryos?
On the scheduled day of FET, the device containing the blastocyst is taken out of the liquid nitrogen and rapidly warmed to 37oC before being washed through a series of solutions to help it to recover. In the hours that follow, the blastocyst should return to its original state ready to be transferred.
For how long can blastocysts be stored?
UK law permits Blastocysts to be stored for up to 10 years, and longer in exceptional circumstances. Freezing stops all activity in the blastocyst cells. This means that the blastocyst does not age and success rates will be in line with your age at the time the blastocyst was stored, regardless of when the thaw and FET takes place.
What proportion of blastocysts survive the thawing process?
The freezing and thawing processes are not without risk and in a small percentage of cases the blastocyst does not survive the thaw. We have refined our techniques over a number of years, and we have excellent survival rates of over 97% for good quality embryos. However, lower quality blastocysts, which did not meet the laboratory criteria for freezing, have a lower chance of survival.
How does one prepare for receiving blastocyst?
The is known as a FET – Frozen Embryo (blastocyst) Transfer. There are two main methods for the lining of your womb to synchronize with the blastocyst transfer. Ultrasound scans are undertaken during the cycle to ensure that the thaw and transfer takes place at the optimal time.
- Natural cycle – this is appropriate for women who have regular cycles and ovulation. Ovulation is detected using testing sticks during a natural menstrual cycle. Following ovulation, the thaw and embryo transfer can be scheduled at the most favourable time for implantation.
- Programmed cycle – this is appropriate for women who do not have regular cycles and involves using medication to prepare the lining of the womb for implantation. Your will be prescribe a personalised plan of medication, which typically involves estradiol tablets or patches to develop the lining of the womb, followed by progesterone to support implantation.
- In both types of cycle progesterone is given in the form of pessaries, which ensure that the lining of the womb is supportive to the blastocyst. This is known as luteal support and continues for either 2 or 12 weeks depending on the protocol that has been recommended for you.
- The success rates are comparable between each protocol; your clinician will advise you which protocol will be best suited to you.
What are the success rates?
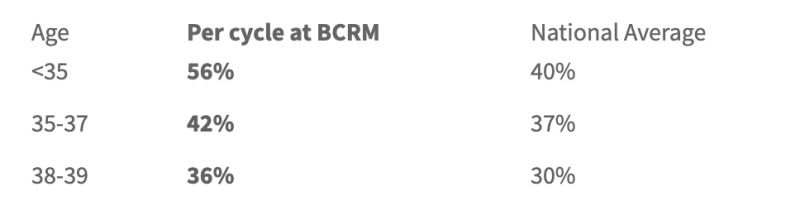
As shown in the Table below, the pregnancy rates at BCRM are higher than the National average (2019 rates published by the HFEA)
What re the risks involved with FET?
- Babies born following a FET are of similar weight to naturally conceived babies than those conceived following fresh IVF cycles. Studies have noted more FET babies can be large for gestational age.
- Recent reports have also suggested that the incidence of pre-eclampsia is increased with frozen embryo transfers when compared with fresh transfers. pre-eclampsia is caused by problems with the placenta and leads to high blood pressure and protein in the urine. Reassuringly the absolute risk remains low, with around 3% of women developing pre-eclampsia following FET compared with 1% after a fresh embryo transfer. The reasons for these changes are not clearly understood.
- The benefits of FETs must always be weighed against the risks, if you have questions or concerns please ask to speak to a member of the clinical or laboratory team