Preimplantation Genetic Testing for Aneuploidy – PGT-A
Dr Amanda Jefferys,
Consultant Gynaecologist and Subspecialist in Reproductive Medicine
What is PGT-A?
PGT-A (Preimplantation Genetic Testing for Aneuploidy) previously known as Preimplantation Genetic Screening (PGS), is a method of screening embryos for chromosomal abnormalities prior to transfer back to the womb at the time of IVF.
How is PGT-A helpful?
It is expected that a proportion of all embryos formed will be chromosomally abnormal (chromosomes being the packages that carry genetic information). These are known as aneuploid embryos. This is true whether the embryo was formed through natural conception or assisted conception (IVF). A chromosomally abnormal embryo is less likely to implant and more likely to result in a miscarriage. Chromosomal abnormalities rarely result in a live-birth and if they do there can be associated health problems for the child. The likelihood of an embryo carrying a chromosomal abnormality increases with age (Fig 1). Typically, in women who are 35-37 50% of embryos will be chromosomally abnormal, this figure rises to 75% in women in the 41-42 age group. This goes some way to explaining the lower pregnancy rates and increased miscarriage rates in women as they get older. PGT-A increases the likelihood of a chromosomally normal (euploid) embryo being transferred back at the time of IVF treatment.
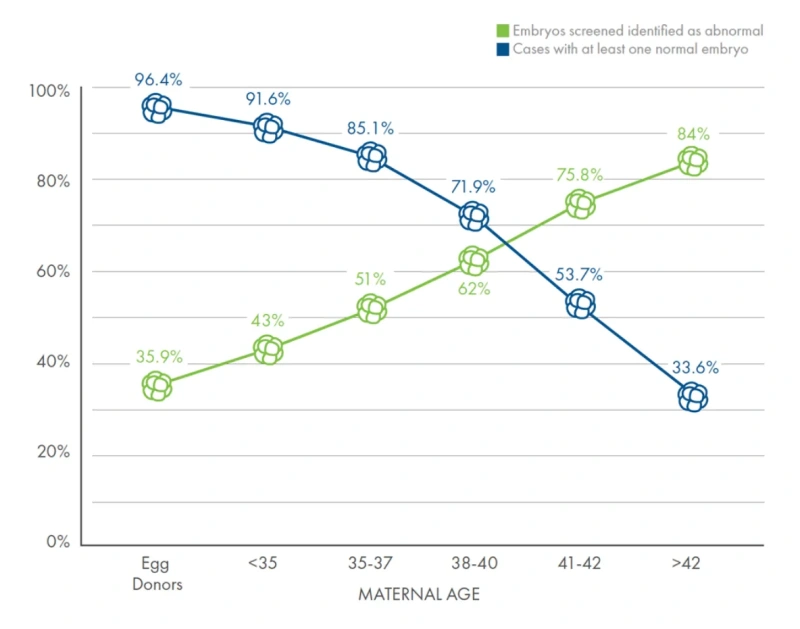
Fig 1 – Provided by Cooper Genomics
Who would benefit from PGT-A?
PGT-A is an option for anybody undergoing assisted conception treatment, however those more likely to benefit from this treatment include:
- Those who have had repeat unsuccessful cycles of assisted conception treatment where no other reason for the failure of the cycle is suspected.
- Women >37 years of age
- Couples with a history of repeat (recurrent) miscarriage
- Couples who have had a previous pregnancy affected by chromosomal abnormalities
What is involved in PGT-A?
Embryos are created using IVF / ICSI in the usual way. Once the embryos have reached the advanced (day 5) embryo stage (also known as the blastocyst stage), a small sample of cells are removed from the outside of the embryo using a microscopic laser, these cells are not essential to the ongoing growth and development of the embryo. The cells are sent for genetic analysis at a genetics laboratory using a technique called Next Generation Sequencing. Meanwhile the blastocysts will be frozen. The results take 2-3 week to come back, a consultation is then arranged with a fertility consultant to discuss these results.
What is the PGT-A process?

Diagram provided by Cooper Genomics
What results might I expect?
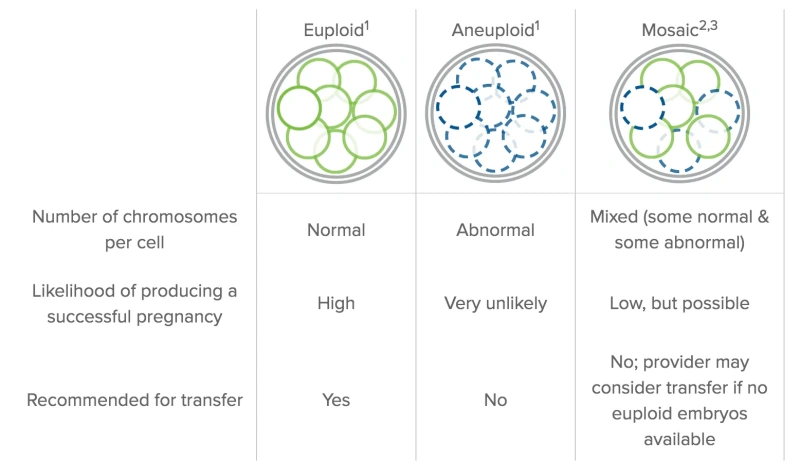
For each embryo one of three results will be received:
- The embryo may be euploid meaning it carries a normal number of chromosomes, these are the embryos that are ok to be transferred.
- The embryo may be aneuploid meaning it carries an abnormal number of chromosomes, it may have an extra chromosome, be missing a chromosome or have an extra set of chromosomes. These embryos would not be considered suitable for transfer as there is a high chance of implantation failure, miscarriage or a chromosomally abnormal baby (in the very unlikely event the pregnancy continues to term) with these embryos.
- The embryo may be a mosaic. This means that some of the cells removed and tested have an abnormal number of chromosomes and some do not. They can result in normal pregnancies although pregnancy and livebirth rates are lower with these embryos. It may if there are no euploid embryos that the fertility consultant advises transfer of a mosaic embryo.
Once a decision has been made as to which embryo(s) should be transferred back a frozen embryo transfer is arranged in either a natural or programmed (medicated) cycle.
What are the risks of having PGT-A?
- No embryos for biopsy. There is a chance that no embryos develop on to the blastocyst stage and therefore that there are no embryos for biopsy and transfer. However, it is very likely that embryos that fail to develop to the blastocyst stage would be chromosomally abnormal.
- Embryo damage. There is a risk of embryos being damaged during the biopsy process meaning they are not suitable for freezing and transfer. This risk is very small (typically less than 1%). Your clinic should be able to advise you of the rates of embryo damage in their centre.
- No aneuploid embryos. There is a chance that all the embryos biopsied are aneuploid and therefore that there is no embryo suitable for transfer. This become more likely as female age increases.
- Risk of misdiagnosis. Unfortunately, tests are rarely 100% accurate and there is a risk of a euploid embryo being incorrectly diagnosed as aneuploid and an aneuploid embryo being diagnosed as being euploid. The chances of this are less than 1%. We would always recommend prenatal screening for chromosomal abnormalities after PGT-A.
- Unfortunately, PGT-A does not guarantee a pregnancy or a healthy live birth nor does it eliminate the risk of miscarriage.
We hope this has been a useful introduction to PGT-A. Please get in touch with the BCRM team if you would like further information.
Dr Amanda Jefferys, Consultant Gynaecologist and Subspecialist in Reproductive Medicine
info@bcrm.org.uk
0117 301 8605
