Why might I undergo PGT-A testing?
We know that chromosomally normal embryos are more likely to result in a successful pregnancy and live birth. PGT-A is a selection tool to increase the likelihood of a healthy ongoing pregnancy but is not a guarantee of pregnancy and does not replace the need for antenatal screening.
PGT-A cannot be used for sex selection purposes, which is illegal in the UK. It is only indicated for genetic/medical reasons. BCRM staff do not know the sex of the embryos when the results are received.
Who is PGT-A suitable for?
PGT-A testing is most likely to benefit those:
- with a history of recurrent miscarriages
- who have had several failed IVF attempts
- who have had previous pregnancies affected by chromosome abnormalities
- over the age of 37
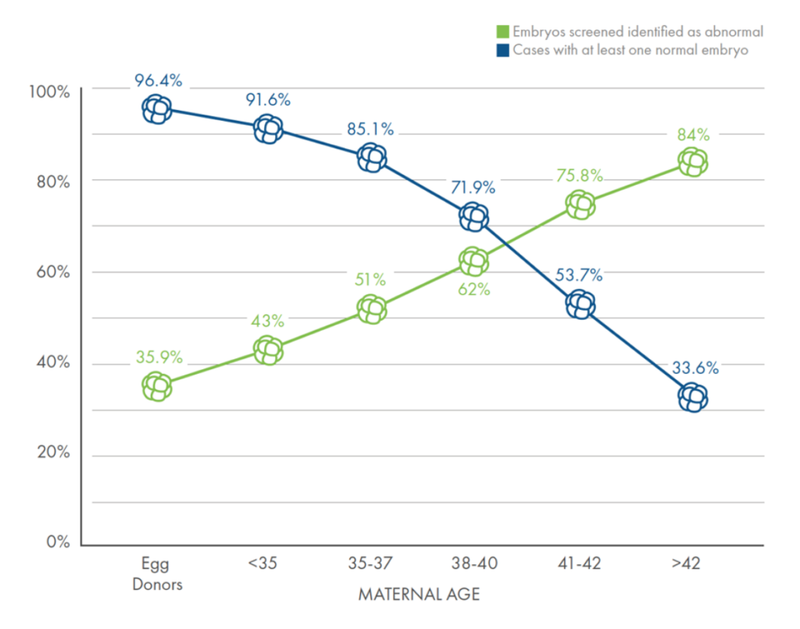
Fig 1 – Provided by Cooper Genomics
Typically in women who are 35-37 50% of embryos will be chromosomally abnormal, this figure rises to 75% in women in the 41-42 age group. This explains the lower pregnancy rates and increased miscarriage rates in women as they get older.
PGT-A testing may reduce these risks, although this has not been conclusively proven. Anyone going through IVF/ICSI treatment can undergo PGT-A testing if they wish.
What test results can I expect?
For each embryo tested, one of three results will be obtained (see fig 2):
- The embryo may be euploid meaning it carries a normal number of chromosomes, these are the embryos that are suitable to be transferred.
- The embryo may be aneuploid meaning it carries an abnormal number of chromosomes. It may have an extra chromosome(s) or be missing a chromosome. These embryos would not be considered suitable for transfer as there is a high chance of implantation failure, miscarriage, or a chromosomally abnormal baby (in the very unlikely event the pregnancy continues to term).
- The embryo may be mosaic. This means that some of the cells removed and tested have an abnormal number of chromosomes and some do not. They can result in normal pregnancies although pregnancy and livebirth rates are lower with these embryos. It there are no euploid embryos to transfer, your fertility consultant may consider transfer of a mosaic embryo.
In most cases, some embryos will be normal and some will be abnormal. However, there is a chance that none of the embryos will be suitable for transfer and this becomes more likely as female age increases.
Less than 5% of embryos tested will fail to give a result. This can be due to the chromosomes degrading before testing, or technical errors. Embryos without a result can still be transferred, but it will not be possible to say whether or not they have a correct number of chromosomes. PGT-A cannot screen against genetic disorders and does not guarantee a child will not be born with a genetic disorder (e.g. Cystic Fibrosis) rather than a chromosomal disorder (e.g. Down’s Syndrome).
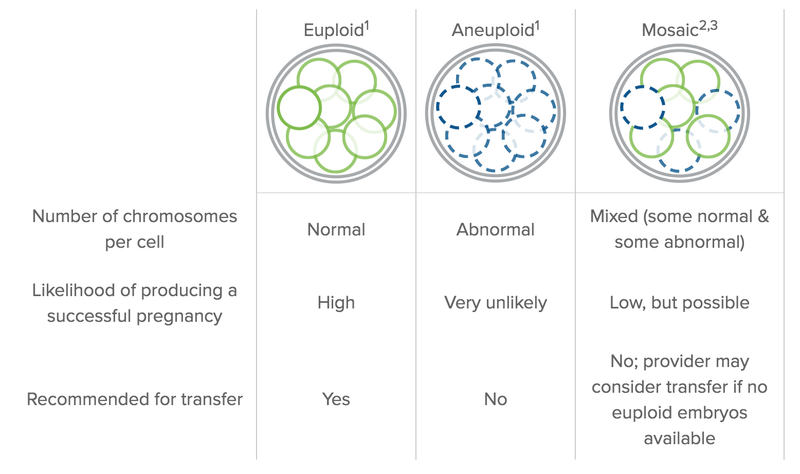
Fig 2 Provided by Cooper Genomics
What are the risks of having PGT-A testing?
- Embryo damage. There is a risk of embryos being damaged during the biopsy process meaning they are not suitable for freezing and transfer. This risk is very small (typically less than 1%).
- Risk of misdiagnosis. Unfortunately, tests are rarely 100% accurate and there is a risk of a euploid embryo being incorrectly diagnosed as aneuploid and an aneuploid embryo being diagnosed as being euploid. The chances of this are less than 1%. We would always recommend prenatal screening for chromosomal abnormalities after PGT-A testing.
Unfortunately, PGT-A testing does not guarantee a pregnancy or a healthy live birth nor does it eliminate the risk of miscarriage
PGT Treatment
The steps you will undergo in PGT testing and treatment
1. Specialist Consultation
All patients will need to have a PGT consultation with one our specialist doctors before embarking on IVF/ICSI treatment with PGT.
2. IVF/ICSI Treatment
You will proceed with a treatment cycle of IVF/ICSI to create embryos for testing, including medication, ultrasound scans, egg collection and fertilisation.
3. Biopsy
An embryologist will be able to advise you on how many blastocysts are suitable for biopsy and collect 5-10 cells from each you wish to test.
4. Testing
The cells will sent to a specialist lab for testing and it will take 2-3 weeks to receive the results. The blastocysts will be frozen while we await the results.
5. Results Consultation
You will have an appointment with your consultant to discuss the results of the genetic screening and they will advise on your next steps, including planning an embryo transfer if appropriate to do so.
6. Embryo Transfer
You will have a Frozen Embryo Transfer (FET) cycle to transfer your euploid embryo.



